The Use of Ciclosporin in Anal Furunculosis

HISTORY AND CLINICAL EXAMINATION
 A five-year-old, female, entire, German Shepherd dog presented at four years of age with an eight-week history of perineal discomfort and a pruritus score of 10/10. Prior to referral, she had previously been treated with short courses of antimicrobials and was receiving 5 mg/kg PO ciclosporin SID, which did not produce an improvement in clinical signs.
A five-year-old, female, entire, German Shepherd dog presented at four years of age with an eight-week history of perineal discomfort and a pruritus score of 10/10. Prior to referral, she had previously been treated with short courses of antimicrobials and was receiving 5 mg/kg PO ciclosporin SID, which did not produce an improvement in clinical signs.
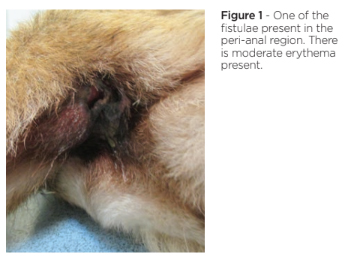
On clinical examination, the dog was found to be underweight with no other general abnormalities present. On examination of the perineal region, there were two peri-anal ulcerated fistulae seen which were associated with a purulent exudate.
DIFFERENTIAL DIAGNOSES
-
Deep pyoderma secondary to anal furunculosis
-
Anal sac disease
-
Anal or rectal neoplasia
-
Secondary anal pruritus with underlying primary hypersensitivity disorder
DIAGNOSTIC TESTS
Cytological examination of the exudate was performed and showed large numbers of neutrophils and a mixed infection with large numbers of coccoid and rod-shaped bacteria, some of which were intracellular. A sterile swab was taken for culture and sensitivity, which showed mixed anaerobes, Gram positive Enterococcus faecalis and Gram negative Escherichia coli.
TREATMENT
 Based on the results of the diagnostic tests performed, the dog was prescribed metronidazole 10 mg/kg SID and cefalexin 20 mg/kg BID for six weeks.
Based on the results of the diagnostic tests performed, the dog was prescribed metronidazole 10 mg/kg SID and cefalexin 20 mg/kg BID for six weeks.
Six weeks on, therapy was switched to liquid ciclosporin at 5mg/kg SID as the owner was having difficulty administering oral capsules. Tramadol was dispensed at 5 mg/kg TID to provide analgesia, as the dog was reported to be depressed and appeared painful when defecating.
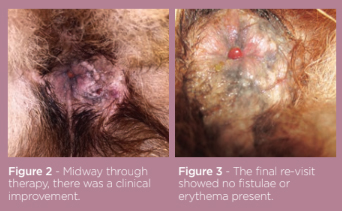
Four weeks on, the pruritus was graded as 5/10 with a vast improvement in the lesions. There was no exudate, the area appeared clean and both fistulae had dramatically reduced in size. Conscious rectal examination was possible, eliciting less pain than previously shown. There was marked thickening to the right anal sac. However, weight loss had continued. Repeated cytology was performed; there were still coccoid and rod-shaped bacteria present although in lower numbers, along with neutrophils. The metronidazole and cefalexin were continued alongside the ciclosporin at the same doses and topical 0.3% tacrolimus cream SID was added.
Four weeks on, there was a superficial pyoderma on the ventrum. A 2% chlorhexidine and 2% miconazole shampoo was added to be used twice weekly. There were other clinical signs displayed, including vomiting and lethargy. Routine haematology and biochemistry was performed which showed no abnormalities. The metronidazole was stopped and the ciclosporin was reduced to 3 mg/kg in response to the vomiting. The topical tacrolimus was stopped at this point. Another four weeks on, the vomiting remained so the ciclosporin was reduced to 1.7 mg/kg. At this point, the dog was referred to the internal medicine department for investigations and was subsequently diagnosed with a chronic enteropathy and treated accordingly.
Six months after first presentation, the dog’s demeanour had markedly improved and the anal furunculosis was in remission. The vomiting had stopped and the ciclosporin was reduced again to 1.6 mg/kg. The cefalexin had been stopped and there was no evidence of continuing infection of the peri-anal region. The fistulae were no longer visible. Ongoing the low dose of ciclosporin and the hypoallergenic food are being given to manage the dog’s disease.
In this case the anal furunculosis was complicated by secondary microbial infection and this needed to be addressed. Some cases of anal furunculosis are also associated with dietary manipulation to help control the skin condition.
SUMMARY
Anal furunculosis is a disease of the perianal skin, anal sacs and mucocutaneous junctions.1 Its pathogenesis is unknown but there is presumed to be an immune-mediated aspect. As in this case, German Shepherd dogs are predisposed to this condition but it can occur in other breeds.2
The disease presents with micro-abscesses within the dermis, which progress to ulcers, and finally fistulae; these can become secondarily infected and can be associated with a purulent discharge as seen in this case.1 It is a painful disease and this can lead to dyschezia, tenesmus and constipation.2 There is a wide range of treatment options, starting with antimicrobial therapy (both oral and topical) for the secondary infections, but being based around immunomodulating or immunosuppressive therapy, ranging from oral and topical glucocorticoids, oral ciclosporin, oral azathioprine and topical tacrolimus.1,2 Some cases benefit from being managed with dietary manipulation in conjunction with medication.


