The Use of HCA in Allergic Otitis Externa
HISTORY AND CLINICAL EXAM
 A 4-year-old female neutered Labrador Retriever dog was presented with an eight-month history of recurrent bilateral otitis. This first manifested as head shaking, scratching around the ears and excessive amounts of otic cerumen. Swabs for bacterial and fungal culture repeatedly isolated Malassezia spp. With each episode of otitis, clinical signs resolved with the use of licensed topical polypharmacy ear medications and oral corticosteroids. However, head shaking and discomfort returned within a few weeks of these medications stopping and the dog was subsequently referred for further investigation.
A 4-year-old female neutered Labrador Retriever dog was presented with an eight-month history of recurrent bilateral otitis. This first manifested as head shaking, scratching around the ears and excessive amounts of otic cerumen. Swabs for bacterial and fungal culture repeatedly isolated Malassezia spp. With each episode of otitis, clinical signs resolved with the use of licensed topical polypharmacy ear medications and oral corticosteroids. However, head shaking and discomfort returned within a few weeks of these medications stopping and the dog was subsequently referred for further investigation.
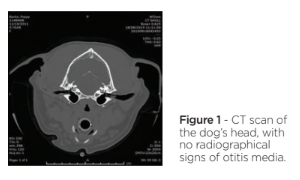
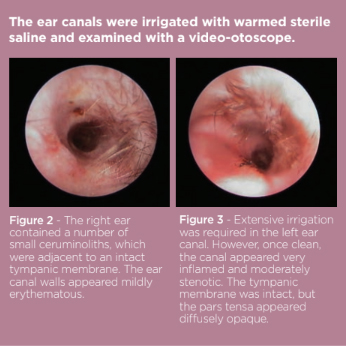
On presentation, general physical examination revealed no significant abnormalities. Dermatological examination demonstrated bilateral otitis with no other skin lesions. The right ear pinna and canal were mildly erythematous but the tympanic membrane was visualised and appeared intact. The left ear pinna was also erythematous, with both the vertical and horizontal sections of canal markedly inflamed. The horizontal canal was also filled with brown waxy exudate obscuring visualisation of the tympanic membrane.
DIFFERENTIALS
- Primary –
- Allergic skin disease
- Ectoparasitism
- Foreign body
- Keratinisation disorder
- Autoimmune disorder
- Secondary-
- Bacterial infection
- Yeast infection
- Perpetuating-
- Otitis Media
- Ear canal stenosis
- Glandular hyperplasia
DIAGNOSTICS
Microscopic examination of otic cerumen failed to reveal signs of ectoparasites. A further sample was collected from both ears for cytological assessment, revealing elevated numbers of neutrophils and large numbers of unipolar budding yeasts (consistent with Malassezia spp.) in the left ear. There were no microbes or inflammatory cells recovered from the right ear.
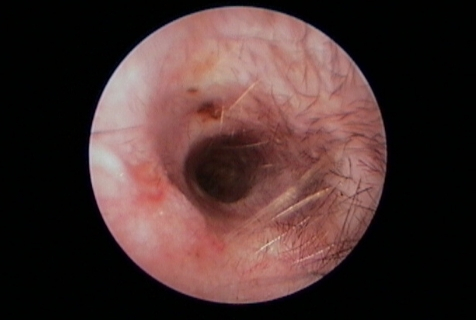
Due to the possibility of perpetuating factors, the dog was anaesthetised for a CT scan of the ear canals and tympanic bullae. However, this did not reveal evidence of otitis media (Figure 1). The ear canals were irrigated with warmed sterile saline and examined with a video-otoscope. (Figure 2, Figure 3).
TREATMENT
To address the secondary infection in the left ear, topical treatment was initiated with once daily HCA/gentamicin/miconazole ear suspension. The owners were instructed to clean both ears twice weekly. A course of oral methyl-prednisolone 0.4mg/kg once daily was prescribed to reduce ear canal inflammation.
The dog returned 3 weeks later and cytological samples confirmed resolution of infection in the left ear. However, both pinnae and canals of both ears still appeared erythematous. Given the persisting ear canal erythema in the absence of microbes, underlying allergic skin disease was considered most likely. A dietary trial (to investigate cutaneous adverse food reaction) was discussed but declined by the owner. Therefore, with inflammation localised to the ears, a solution of HCA 0.584mg/ml spray, diluted 1:4 with 0.9% sodium chloride, was formulated. The owners were instructed to administer 0.5mls to both ears on alternate days, alongside continued ear cleaning.
The dog returned 4 weeks later making good progress, with resolution of head shaking and ear scratching. Otoscopy revealed clean ear canals with reduced erythema and reduced stenosis in the left ear. Cytological samples demonstrated an absence of microbes. The diluted HCA solution was continued twice weekly with ear cleaning once weekly.
The dog returned 3 weeks later. Both ear canals appeared clean, patent and no erythema seen. Cytology revealed no microbes. The owners were advised to continue the same topical regimen, and, six months on, the dog’s otitis remains in remission.

DISCUSSION
Otitis in dogs is a multifactorial problem, with primary and secondary causes of inflammation, predisposing factors and perpetuating factors.¹´² A successful outcome relies on managing all factors. When allergic skin disease is suspected as the primary trigger, control over this inflammation is vital to prevent further relapses of infection and chronic perpetuating factors developing.
Allergic skin disease in dogs can manifest solely with otitis, and these cases lend themselves to topical treatment. HCA 0.584mg/ml spray has been shown in numerous studies to be an effective topical treatment for atopic dermatitis.³¯⁵′⁷′⁸ It was able to decrease lesion scores by >50% in 11 of 15 dogs after 28 days of treatment, and there were no changes to complete blood count, serum biochemistry or ACTH stimulation testing for up to 70 days.⁴
There are no licensed topical corticosteroid-only ear products for dogs in the UK, so HCA 0.584mg/ml spray use in the ear canals is off license and based on the prescribing cascade. The decision to dilute the HCA 0.584mg/ml spray here was purely based on the desire to limit the amount of drug being used. However, undiluted HCA 0.584mg/ml spray has been administered to the ear canals by some clinicians.⁹
The dog in the present case tolerated the treatment well. The allergic otitis was successfully controlled in long term remission with the intermittent use of ear cleaner and topical off-license corticosteroid solution, preventing the need for systemic medications.


